
General information
A disease of the human musculoskeletal system, such as osteochondrosis, is essentially a degeneration of articular cartilage and nearby bone tissue with a mixture of vessels, muscles and nerve endings adjacent to the pathological process. In principle, this term can refer to a number of osteoarticular pathologies of different localization, including joints of the extremities, but in most cases it is used to indicate degenerative-dystrophic changes in the structure of the direct spine and, above all, the intervertebral discs.
As a result of the development of intervertebral osteochondrosis, the human body loses its shock-absorbing qualities, mobility and elasticity. In general, this disease of the spine is very common, and in most people there is a different degree of severity up to 40 years. In clinical practice, cervical, lumbar and thoracic osteochondrosis and mixed forms differ depending on the affected segment of the lumbar spine. is considered the most difficult.
Osteochondrosis of the thoracic spine, which will be discussed in this article, is the rarest form of this pathology, especially due to the anatomical structure of the upper part of the human skeleton. Thus, the skeletal-cartilage system in the thoracic region consists of 12 vertebrae connected between the ribs and joints adjacent to a relatively monolithic sternum with anterior ends. Such a skeletal structure is sufficient for a rigid and strong frame that protects the organs of the cavity (heart, lungs) from damage. In addition, the vertebrae of this segment of the spine are characterized by a small height and a significant length of spinous processes, which gives them the appearance of spaced plates. All this, together, limits the mobility of this part of the spine and the negative impact of physical activity on it, protects the intervertebral discs from destruction.
As a lower cause of thoracic osteochondrosis in humans, physiological kyphosis (natural backward curvature of the spine) occurs in this region compared to lumbar and cervical osteochondrosis, due to the fact that most of the external load falls on the anterior and lateral parts of the spine and discs. With the development of a pathological process in the segment of spinal movement, these areas are primarily degeneratively affected, but pain is most often not observed due to the absence of nerve endings and spinal cord membranes. However, in some cases, adverse changes in the thoracic segment of the spine affected the discs and the posterior fragments of the vertebrae and / or spinal-costal joints, leading to compression of the spinal nerve roots. Under such conditions, osteochondrosis of the spine occurs with the already existing radical syndrome, accompanied by pain of various localizations (sometimes very distant) and dysfunction of many organs of the human body (liver, lungs, pancreas, heart, etc. ).
Because of such incomprehensible and various manifestations of thoracic osteochondrosis, doctors often call this pathological form "chameleon disease" because it can disguise itself as a symptom of respiratory and digestive diseases, heart muscle, etc. In this situation, a properly differentiated diagnosis is very important, which will help to determine the symptoms and treatment of osteochondrosis of the thoracic spine with various specific studies.
The tactics and effectiveness of complementary therapy will depend on the degree of development of degenerative-dystrophic process in the tissues of the spine. Although it is important to improve the patient's condition after recognizing the pathology in the early stages of development, it is quite possible with the help of physiotherapy techniques and exercise therapy, but in case of late detection, a complex surgery may be required. Therefore, vertebrologists recommend that you seek professional help as soon as possible for any frequent and / or prolonged back pain.
Pathogenesis
The occurrence of osteochondrosis of the sternum in women and men is practically the same, because there is no sexual tendency to the onset of intervertebral disc degeneration in the pathogenesis of this disease. However, many years of clinical experience in the treatment of osteochondrosis show that the first symptoms in men appear at an earlier age than similar negative symptoms in women. In particular, due to the fact that it is osteochondral, the tissues of the female body up to a certain age are protected by the hormone estrogen, a decrease in levels during climacteric transformations leads to problems with the spine.
According to statistical evidence, in general, most older people have intervertebral osteochondrosis of varying severity, which automatically belongs to the group of age-related diseases. Meanwhile, the latter is followed by a significant "rejuvenation" until the onset of this pathology in preschool age. Therefore, to date, it has not been possible to determine the exact etiology and initial pathogenesis of spinal osteochondrosis. At one time, more than a dozen theories of its origin and development, including hormonal, infectious, mechanical, vascular, hereditary, allergic, and others, were developed, but none were fully confirmed in practice.
Today, doctors explain the occurrence of osteochondrosis by the sum of the complementary adverse effects on the spinal tissues, among which there is a constant overload in one or more spinal movements. segments consisting of two adjacent vertebrae (upper and lower) and a disc located in the middle of them. Paradoxically, such a load can be the result of both excessive physical activity of the spine, and the result is a long-term finding in an unnatural position. For example, working or reading for long periods of time while sitting at a table is one of the main factors in the development of degenerative-dystrophic changes in the intervertebral structure. disk.
The initial formation or exacerbation of osteochondrosis of the sternum can be influenced by poor nutrition, uneven development of the dorsal and pectoral muscles, overweight (obesity), pathology of the lower extremities (eg, straight legs), back injuries, etc. Segmental circulatory disorders play an important role in the pathogenesis of this disease, which leads to dehydration of the pulpous (gelatinous) nucleus, which in turn leads to loss of amortization of the intervertebral disc, changes in the loads on the surrounding fibrous ring and the gradual destruction of this spinal cord.
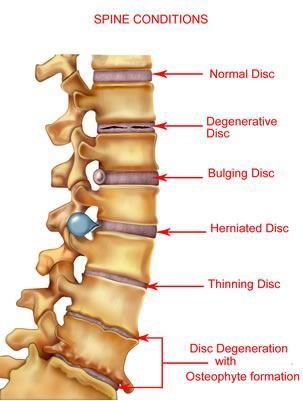
Thoracic osteochondrosis goes through 4 stages of development, each of which is characterized by its own anatomical and morphological changes in the structure of the disc, adjacent vertebrae and facet. joints. In addition, the negative metamorphoses that occur with this disease can directly affect other nearby tissues (muscle, blood vessels, connective tissue) or indirectly affect the functioning of distant organs and systems of the human body. (intestine, heart, lungs, etc. ).
First degree
In the early stages of thoracic osteochondrosis, micro-cracks appear in the inner membrane of the fibrous ring, where the nuclear pulposus gradually begins to penetrate, irritating the nerve endings in the distal layers of the fibrous region. rings and longitudinally in the back garden. At this stage in the development of the disease, the patient may already feel pain directly in the middle of the lower back or appear painful in the heart area. A feeling of convulsive contraction may follow. in the dorsal muscles.
Second degree
Grade 2 osteochondrosis of the sternum is characterized by further destruction of the ring fibrosis, accompanied by instability of the spine as a result of excessive mobility of the affected vertebrae. From the 2nd stage of the development of pain pathology, the sensations intensify and may continue dorsalgia (minor persistent pain aggravated by lumbar movements) or dorsago (severe pain that occurs sharply against the background of prolonged stay in one position).
Third degree
In the third stage of thoracic osteochondrosis, there is a complete rupture of the annulus fibrosus structure with the protrusion of the pulposus nucleus and the formation of an intervertebral hernia. Often such formations occur in the vertebral direction, leading to compression of the spinal cord, spinal nerves and adjacent vessels. These include radicular syndrome (radiation pain to various parts of the body), thoracolgia (severe pain in the back of the sternum, similar to the heart), myelopathy (sensory and motor disorders), and other neurological and muscular-tonic symptoms. Fixed chest pain, scoliosis or kyphoscoliosis can begin at this stage.
Fourth degree
In the final stage of thoracic osteochondrosis, degenerative processes spread to the jaw and jaundice, other tissues of the spine and nearby muscles. Intervertebral disc dystrophy lasts until the development of scarring and more fibrosis. Deformative arthrosis develops in the lumbar and intervertebral joints, osteophytes (bone growths) are formed in the vertebral processes. The clinical picture at this stage of the disease can be very diverse, as the degree of damage to individual discs often varies. In uncomplicated osteochondrosis, fibrosis of the problem disc may indicate a transition to a stable remission of the disease, but with some degree of loss of normal functionality. spinal column.
Reasons
Osteochondrosis of the chest in men and women can develop due to the following predisposing factors:
- natural physiological aging process accompanied by age-related changes in the structure of bone and cartilage tissue of the spine;
- genetic predisposition to abnormal formation of spinal movement segments;
- a physically inactive lifestyle that causes dystrophy of the back muscles;
- Strong sports involving excessive mechanical stress on the spine (primarily weightlifting);
- spinal cord injuries (even those that happened in the distant past);
- endocrine diseases in the human body, impaired nutrition of spinal tissues;
- significantly above normal body weight (obesity);
- harmful diet (vitamin, mineral and fluid deficiency);
- spinal pathology with unnatural flexion;
- imbalance in muscle frame development;
- long-term work or sitting with the body bent;
- physically difficult working conditions (always incorrect lifting of weights);
- serious metabolic diseases;
- other diseases of the lower extremities affecting the redistribution of loads around the straight legs and waist;
- vascular diseases that disrupt the posterior blood supply;
- severe infectious, allergic and autoimmune processes;
- frequent hypothermia;
- stressful situations and nervous exhaustion;
- bad habits and smoking.
Symptoms of thoracic osteochondrosis
Symptoms of thoracic osteochondrosis may not be of direct concern to the patient for a long time due to the above-mentioned structural features of this part of the spine, and may appear only if the pathological process spreads laterally. and / or the posterior parts of the affected spinal movement segments and the progression of the disease to the second or third degree. In general, all symptoms of thoracic osteochondrosis are expressed in the form of vertebral syndromes (painful effects are directly related to functional disorders in the bone and cartilage tissue of the spine) and extravertebral or compression syndromes (adverse events caused by pathological impulses from the problem segment of the spine).
Vertebral syndromes
The vertebral symptoms of osteochondrosis of the spinal segment are mainly manifested by two pain syndromes called dorsago and dorsalgia.
Dorsago
It is an acute and sudden pain attack called "lumbago" that is localized in the interstitial space and can occur at any time. In most cases, patients with dorsago syndrome are in a sitting position with the body leaning forward and the body position changing dramatically. Patients describe the moment of the attack as a "dagger blow" accompanied by a sharp spasm of the spinal muscles. In addition to severe pain, subjective sensations with the dorsal are expressed by shortness of breath and significant restriction of freedom of movement in the thoracic region of the back. Exacerbation of osteochondrosis, similar to periodic attacks, can last up to two weeks.
Dorsalgia
This syndrome differs from the previous ones by the gradual development of anxious and painful feelings that can increase in two to three weeks. The pain itself with dorsalgia is not so pronounced, but it is a constant feeling of anxiety that causes its long-term existence. The dorsal muscles, as well as the dorsal muscles, are subjected to significant stress, which can cause the patient to feel shortness of breath. Back pain increases with trunk movements (especially when bending), deep breathing, coughing, etc. Upper dorsalgia (the main localization of adverse events in the cervicothoracic segment of the spine) and lower dorsalgia (the main localization of adverse events is the thoracolumbar segment of the spine).
Extravertebral syndromes
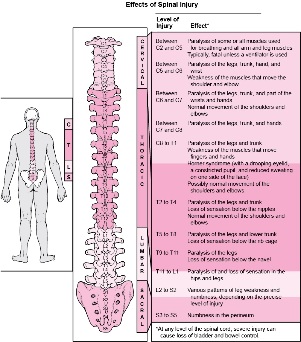
Extravertebral syndromes of thoracic osteochondrosis can be very different due to the large extent of this part of the spine, which greatly complicates the correct diagnosis of the disease. These are caused by mechanical compression of the corresponding nerve roots, nearby blood vessels or the spinal cord itself. Compression symptoms are generally similar in men and women, and differ only when pathological impulses are transmitted during sexual intercourse (for example, erectile dysfunction is sometimes noted in men against the background of the disease). In almost all cases, extravertebral symptoms are more often caused by already formed intervertebral hernias, which are seen below. thoracic regions, but in principle can occur in any spinal-motor segment from vertebra D1 to vertebra D12. As you can see in the figure below, the process of localization of osteochondrosis, which is associated with pathology, with characteristic adverse manifestations of certain systems and organs of the human body.
Radical syndromes
Within the compression symptoms of thoracic osteochondrosis, radicular syndromes provoked by compression of nerve endings in one or another segment of the spine are the most common and obvious. Depending on the concentration, patients may have problems with the following painful events:
- In the case of a violation in the region of the T1 vertebra - from the segment of the upper thoracic spine movement, painful sensations and paresthesias most often along the suprascapular zone to the area of one of the armpits to the elbow joint;
- In the case of T2-T6 disorders in the spinal area - pain such as intercostal neuralgia may extend along the anterior region of this part of the spine and may cover the axillary and scapular zones within the semicircle, as well as 2-6 intercostal spaces;
- In the case of a violation of the T7-T8 vertebrae - lumbar pain, mainly spreads from the lower level of the shoulder blades of the spine-costal joints to the upper part of the expensive arch and affects the epigastric region. muscle protection (strong muscle tension);
- In case of spinal cord injury in the T9-T10 region - intercostal neuralgia, extends from the lower thoracic spine movement segments to the lower part of the arch and then to the umbilical region, changes the tone of the middle abdominal muscles;
- In the case of disorders of the T11-T12 vertebrae - the pain also extends from the lower thoracic spinal segments and reaches the groin area along the hypogastric (below the stomach) and the corresponding lateral zones of the chest.
In addition to pain, radical syndromes of thoracic osteochondrosis are often accompanied by adverse symptoms of the abdominal cavity and / or internal organs of the chest. Moreover, in some cases, such symptoms are so similar to the pathological manifestations of other diseases that it is practically impossible to accurately identify their affiliation without targeted research. For example, an inappropriate behavior is described in the medical literature as appendectomy (surgery to remove an appendix) according to the clinic of acute appendicitis, which appears to be one of the most obvious syndromes of osteochondrosis.
Thus, when the osteochondrosis process is localized in the upper part of the spine (T1 to T4), patients may experience frequently received pain and / or various discomforts in the esophagus or esophagus. the presence of a foreign body. Such feelings are often paroxysmal (sometimes persistent) and are exacerbated by a serious load on the problem area of the lower back. Sometimes the manifestations of radicular syndrome in the upper chest segment are mixed with symptoms of obstructive bronchitis or pneumonia, because a reflex cough with osteochondrosis of the chest and chest pain resembles the symptoms of this group of diseases. In addition, the intensity of chest pain in the form of thoracic angina pectoris, pulmonary thromboembolism, myocardial infarction and other similar pathologies of a serious nature that require detailed differential analysis from physicians.Patients with osteochondrosis of the middle thoracic segment of the spine (T5 - T7) most often experience discomfort and pain in the solar plexus and stomach, called vertebral gastralgia. On the defeat of spinal movement segments T8-T9, it is possible to develop pain in the duodenum - vertebral duodenalgia. . . The intensity of both different and different or other painful sensations can vary from mild and "painful" to extremely sharp. In the case of sudden movements of the body, as a rule, exacerbated by prolonged stay of the body in one position (sitting at a table, lying on the back, etc. ), as well as the moment of sneezing or coughing. Often these pains are accompanied by paresthesia. in the middle of the abdominal wall (numbness, tingling, burning).
With radical manifestations of osteochondrosis in the lower part of the spine (T8 to T12), some patients may complain of pain in the lower abdomen, mimicking intestinal disorders. or pathological. Sometimes the pain spreads to the gallbladder and is localized in the back of the right hypochondrium. Less often, patients experience pain similar to the pathological clinic of the bladder in the suprapubic region. As before, the nature of this type of pain can vary over a wide range (from mild to severe) and can be exacerbated by prolonged physical or static stress on the spine, sneezing, coughing, and so on. grows with.
Compression myelopathy
This compression syndrome of thoracic osteochondrosis is very rare and is caused by compression of the spinal cord directly by an intervertebral hernia. . . . Initially, the characteristic symptom formation is expressed by local pain in the corresponding area of the back or lumbar pain in the problem area, as well as a feeling of weakness and / or numbness in the legs. With progression, the pain intensifies, which can affect the lower extremities, is felt significantly in the intercostal space, abdominal organs, groin area and lower extremities. In severe cases of compression myelopathy may develop pelvic organ dysfunction, which leads to disruption of the processes of defecation and / or urinary excretion. In addition, spastic paresis can be as severe as superficial and deep paresthesias and sensory disturbances. one or both feet.
Vascular Compression
Compression of blood vessels adjacent to the thoracic segment of the spine leads to myelochemia, as a result of which the blood supply is disrupted, and therefore the spinal cord is not properly nourished. Manifestations of this syndrome are, in fact, a complete repetition of the symptoms of compression myelopathy, and are mainly characterized by loss of sensation and decreased functionality in the lower extremities, along with pelvic disorders. Patients often describe this problem with the phrase - "legs do not reach. "
Vegetative syndromes
In some cases, with thoracic osteochondrosis, the autonomic nerve nodes (ganglia) are damaged, resulting in a variety of adverse symptoms. These can be various paresthesias. , itching in the problem ganglion area and changes in skin pigmentation, burning pain in half of the body, local temperature disorders, muscle hyper or shedding, dysfunction of limbs or internal organs, etc. Therefore, these visceral vertebrogenic symptoms are similar to the manifestations of radicular syndromes, but differ from them in the absence of clear localization and the presence of secretory and motor disorders. When a zodiac sign is involved in a pathological process, there may be abnormalities in a node, arms, upper chest and heart that affect the upper thoracic vertebrae. In case of damage to the lower thoracic ganglion, functional disorders can occur in the pelvic, abdominal and thoracic organs, as well as trophic changes in the lower extremities and the rest of the body.



































